Bridging the Gap Between Hospital and Home: Ensuring Smooth Transitions in Healthcare
At Agape Family Healthcare Services, we recognize that healing doesn’t end at discharge. That’s why our care model is built to bridge the gap. Skilled nursing ensures medications are taken correctly. Personal care assistants help with mobility, meals, and hygiene. Companion caregivers ease loneliness, reducing the stress that can slow recovery. Programs like CCSP/Source and GAPP provide structured support for patients with long-term or specialized needs.
10/3/20254 min read

Understanding the Vulnerability of Discharge
The transition from hospital to home represents a critical period for patients, marked by a significant vulnerability that can impact their recovery journey. During this phase, patients frequently face a variety of challenges that can complicate their post-discharge experience. One of the most pressing issues is the change in medication; patients often receive new prescriptions or have their dosages altered, leading to potential confusion and the risk of non-compliance. Mismanagement of medication can result in adverse health outcomes, including increased chances of hospital readmission.
Additionally, the shift from a structured hospital environment to the less regulated home setting can create emotional and logistical hurdles for recovering patients. The hospital typically offers a regimented routine and constant care, whereas home care requires patients to adapt to their own schedules, which can lead to feelings of anxiety and isolation. These emotional challenges can exacerbate physical health issues and hinder recovery.
Statistics reveal the seriousness of these challenges; approximately 30% of patients discharged from the hospital are readmitted within 30 days, often due to inadequate support and communication during the transition. Ensuring that patients have access to adequate resources, such as follow-up care, educational materials about their conditions, and a support network of family or friends, plays a crucial role in mitigating these risks. A well-organized discharge plan that includes clear instructions and follow-up appointments can dramatically improve post-discharge outcomes, allowing patients to navigate this period more effectively.
In recognition of the complexities surrounding hospital discharge, healthcare providers must prioritize communication and support systems. By addressing the emotional, logistical, and medical challenges associated with the transition from hospital to home, the healthcare system can help reduce readmission rates and improve patient satisfaction.
Agape Family Healthcare Services' Comprehensive Care Model
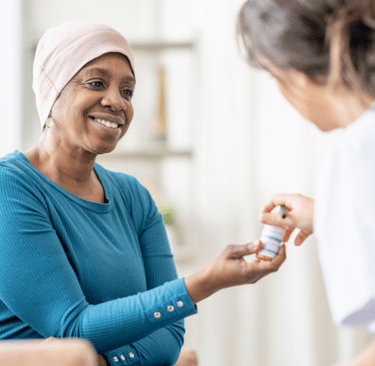
Agape Family Healthcare Services employs a comprehensive care model designed to facilitate seamless transitions for patients reintegrating into their homes after hospital stays. Central to this model is the collaboration of skilled nursing professionals, personal care assistants, and companion caregivers, each contributing their unique expertise to ensure continuity and quality of care.
The role of skilled nursing is pivotal in this model; these professionals provide vital medical support that includes medication management, wound care, and health monitoring. Their presence ensures that complex medical needs are addressed promptly, reducing the risk of complications that may arise during the transition period. By conducting regular assessments, skilled nurses can adjust care plans as necessary, coordinating closely with physicians to maintain a patient’s health trajectory.
Complementing the skilled nursing staff, personal care assistants are crucial for addressing the daily living needs of patients. They assist with tasks such as bathing, dressing, and grooming. This assistance helps promote independence, allowing patients to regain their confidence and comfort in home settings. Additionally, personal care assistants can support medication adherence by prompting patients to take medications as prescribed and observing any potential side effects.
Companion caregivers further enrich the care model by providing emotional support and companionship. They play a vital role in enhancing the overall well-being of patients, helping alleviate feelings of isolation and anxiety that may accompany recovery. Their engagement can take many forms, including meal preparation, light housekeeping, and recreational activities designed to promote mental and emotional health.
Through this holistic approach, Agape Family Healthcare Services ensures successful transitions from hospital to home. By focusing on the medical, personal, and emotional needs of patients, they provide a comprehensive network of support that empowers individuals on their path to recovery.
Programs Designed to Support Seamless Transitions
In today's healthcare landscape, ensuring a seamless transition from hospital to home is critical for patient well-being. Various programs have been established to facilitate this transition and support individuals as they navigate their healthcare journey. Notable among these are the Community Care Services Program (CCSP) and the Service Options Using Resources in a Community Environment (SOURCE). These initiatives are tailored to offer integrated care solutions that empower patients to manage their healthcare needs effectively.
The CCSP is designed to provide alternatives to institutional care for individuals needing assistance with daily living activities. This program offers services such as personal care, home health assistance, and homemaker services, aimed at enhancing a patient's independence in a home setting. Eligibility for CCSP typically includes individuals of all ages who require nursing facility level care but choose to live at home. By fostering patient autonomy, CCSP plays a pivotal role in bridging the gap between hospital care and at-home support.
Similarly, the SOURCE program provides comprehensive support to individuals with varying levels of disabilities, enabling them to remain in their communities rather than transition to long-term care facilities. This program also encompasses essential services, including case management, therapy, and transportation assistance. Eligibility criteria for SOURCE are generally inclusive, allowing a wide range of patients to benefit from its resources. By ensuring individuals have access to necessary support while still engaging in their communities, SOURCE significantly contributes to effective healthcare transitions.
Success stories from these programs highlight their impact. For instance, a patient transitioning from a hospital stay for a chronic condition was able to access services through CCSP, resulting in improved health outcomes and quality of life at home. Such case studies serve as a testament to the efficacy of these programs in facilitating seamless transitions, reinforcing the importance of integrated care approaches in modern healthcare.
The Role of Families and Caregivers in the Recovery Process
The involvement of families and caregivers is crucial in the recovery process post-hospital discharge. These individuals not only provide emotional support, but they also play an essential role in the physical well-being of the patient. Transitioning from a hospital setting to home can be a daunting experience for many patients, and having a robust support system significantly aids in this process. Families and caregivers need to be well-prepared to assist their loved ones as they navigate recovery.
Effective communication is a cornerstone of successful recovery. Families should establish open lines of dialogue with healthcare professionals prior to discharge. This can help them gain a clear understanding of the patient's medical condition, required medications, and necessary follow-up appointments. Setting up a structured care plan that outlines daily tasks and responsibilities can foster collaboration and minimize misunderstandings. For instance, documenting medication schedules and outlining which symptoms to monitor can empower families to take a proactive role in care.
Utilizing available resources is another key strategy. Hospitals often provide materials that guide families on post-discharge care, including instructions for wound care, dietary changes, and signs of potential complications. Families can also benefit from connecting with community resources, such as support groups or rehabilitation services, which can provide additional assistance in the recovery journey.
Moreover, the emotional and psychological aspects of recovery cannot be overlooked. Strong, supportive relationships between patients and their families can create a positive healing environment, ultimately impacting patient outcomes. Understanding the patient’s emotional needs, maintaining regular check-ins, and fostering patience can greatly enhance recovery experiences. In conclusion, the involvement of families and caregivers is indispensable for facilitating smooth transitions and promoting recovery after hospital discharge.
corporate@afhcs.com
470-982-CARE (2273)
Follow Us
6470 E Johns Crossing Ste 100
Johns Creek, GA 30097 USA
Fax: (470) 819-5215
Contact Us
Follow us on social media to get the latest updates about our services and care packages.
